Closing the loop: Why clinical trial results matter to participants

Imagine you take part in a clinical trial, you attend all the clinic visits, undergo numerous tests and assessments, and adhere to your treatment schedule, only to never hear about the results of the trial. Despite 98% of people who participate in clinical trials saying that they’d like to know the outcome of the research, most never do.1
To encourage the dissemination of trial findings, organisations such as the Health Research Authority (HRA) and the World Medical Association (WMA) have published guidelines on the communication of trial results, including recommendations on how to maximise patient and public involvement at every step of the research. Even with these policies and guidelines in place, little is happening to make sure that clinical research findings are making their way to those who want them.2
There are several reasons why study results are often not distributed to participants. Trial teams have reported that one of the greatest barriers to disseminating results is uncertainty around when, what and how to share results with trial participants.3 There is often a lack of initial planning to establish effective processes for easily contacting participants after their involvement in the study has ended. Additionally, it can be challenging to create and get approval for content that is suitable for the entire audience. Researchers also need to be cautious of oversimplifying results to avoid knowledge gaps and missed information when sharing results.4
Why is it important to update participants post-trial?
The number of people taking part in clinical trials is steadily increasing.2 The rise in participation has the potential to change healthcare for the better, so long as the findings reach the right audiences. These include the policymakers who can drive change, the healthcare professionals who deliver the services, and the patients who use them.2
Making sure that research participants know the results of the research that they were a part of is a crucial part of the process. Sharing this information is important for several reasons.
- It shows respect for their time and contribution
People who join clinical research studies often do so out of a want to help advance the science and improve future treatments for a particular medical condition or disease. Sharing the results with participants shows respect for their value and contribution to the research.5,6 - The information could help influence future health-related decisions
One of the key contributing factors to improved health outcomes is having access to health information.7 Getting information about the safety and effectiveness of the treatment studied in a clinical trial could have a real-life impact on the health and health-related decisions of those who took part. - It creates a sense of partnership between participants and researchers
Sharing research findings with participants can help to create a feeling of collaboration between the researchers and the participants. Opening up the research process and creating transparency can empower participants and may encourage participation in future clinical trials.6
What do participants want to know?
More recent exploration of this topic has found that the answer to the ‘what’ is relatively straightforward. Usually, participants don't need or want all the technical details of the trial. They just want to know the main results. For most, a simple summary in everyday language is enough.1
While the style of communication, tone of voice and method of dissemination will vary depending on the audience,8 seven core points should be covered when sending results to participants.
These are:1,9
- Why was the study needed?
- Which medicines or treatments were studied?
- How was the study carried out?
- What did the trial find?
- Were there any unwanted effects?
- What effect will the trial results have on current practice?
- How can I find out more?
While there is some debate about the necessity of including an explicit 'Thank you' message in the materials, acknowledging participants' commitment and altruism is important for showing appreciation and respect for their contribution.9,10
How do participants want to receive updates?
Knowing the audience
It is important to know whether a participant wants to be actively informed of the trial results, or whether they would like to be left out of updates. This can be easily identified early in the participants’ involvement, included as an item on the Informed Consent Form. Any participants who don’t want to receive trial updates should be informed that the results can be found online, from which date, and where they can find them.
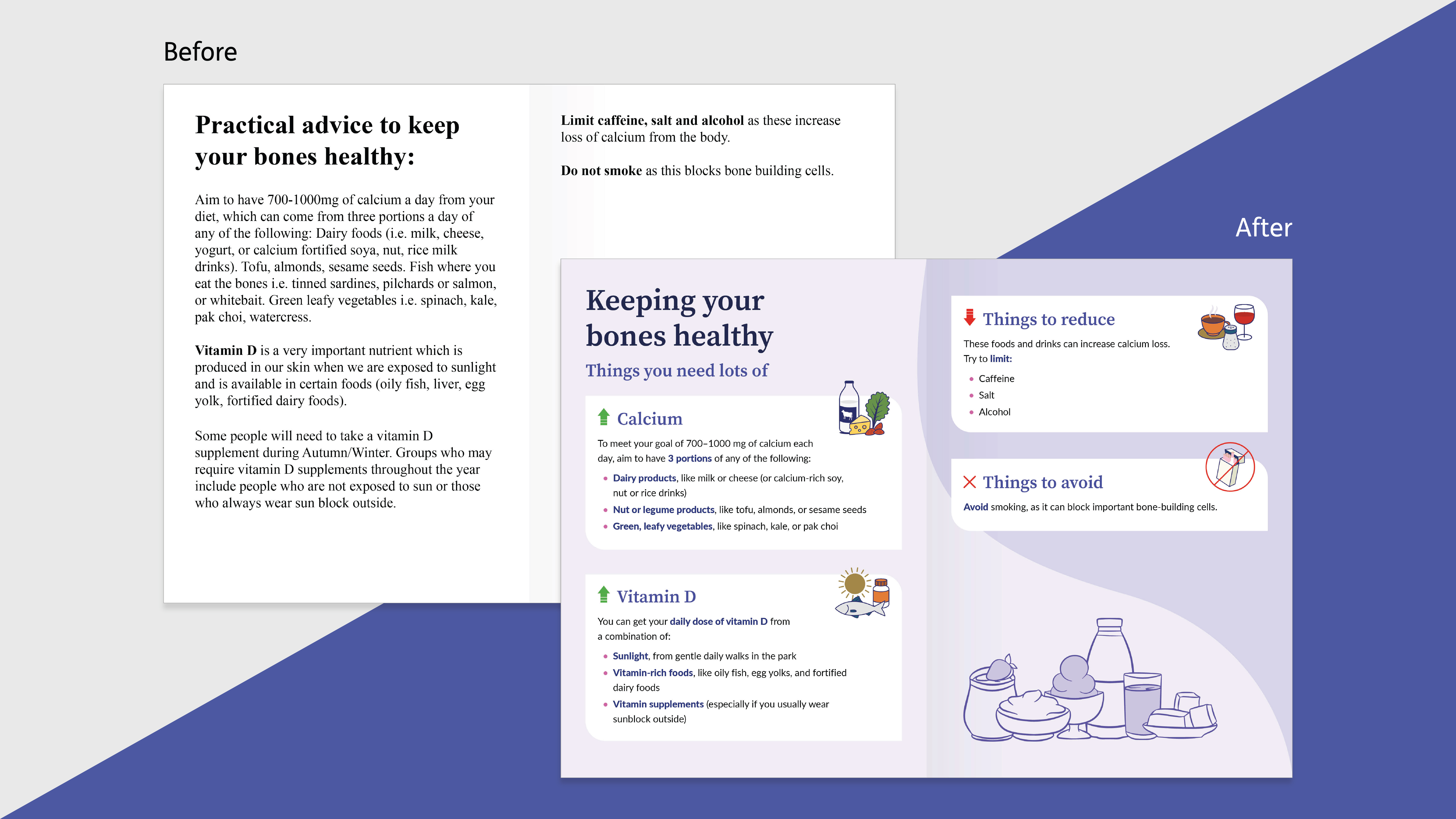
Using the right language
It's important that lay summaries of trial results are written in language that readers can easily understand and engage with. This means that all complex details about the trial and its results need to be translated using simple, everyday language that is accessible to people with all levels of health literacy.11 The best way to achieve this is to use conversational language – in other words, write how you would talk to the target audience.
Language can be kept conversational by:
- Using short words, sentences and paragraphs
- Using active rather than passive voice
- Not using any technical or scientific language
- Putting medical terms in brackets, leading with a lay-language alternative
- Using neutral, non-promotional language11
Local language
Right now, most summaries that are provided are written in English.1 They are often too long and complicated, making them hard to understand even for native English speakers. This also means they are not helpful for people who don't speak English.11 But trial participants want more. In non-English speaking countries, nine out of ten participants would prefer to receive trial results and updates in their own language.1 Trial teams should prioritise translating materials to the local languages of all countries involved in the research. This way, everyone who wants to see the results can understand them and be included.
When to provide results and updates
The best time to share findings depends on the study. For some studies with multiple phases or lots of different outcomes, it may be most helpful to share updates throughout the project or at the end of each phase. This kind of interim updating will be important in clinical trials involving gene therapies, where the gap between the end of the participant’s involvement and the end of the study is long.12 In these cases, it’s important to give participants some information when they finish their part as well as provide the final overall results. Sending regular newsletters or short update bulletins can help to keep the participants engaged and connected to the research.8
Other shorter or less complex studies may only have results disseminated once at the end.
How to disseminate results
The best way to share results depends on the study and the participants. Different approaches will engage different groups. However, sharing trial results by email is often the best method due to its convenience, directness and accessibility for participants.1 Understanding how the audience prefers to receive information can help ensure that the results are shared effectively and reach as many people as possible. Including public and patient involvement at the planning stage can help to provide valuable insights about the specific group of participants in the trial.
The most common ways to present trial updates and results are by:
- Newsletter
- Information sheet
- Study-specific websites or microsites
- Study-specific social media accounts8
Whether results are shared electronically, or created as physical handouts, they should be written in conversational language and include simple graphs and illustrations to help present any numerical data.
What have we learned?
We know that for the most part, clinical trial participants want to be updated with trial results, findings and news updates. Still, there is a discrepancy between the demand and the delivery.
Keeping trial participants informed about the outcomes of the research they were part of shows respect for their time and effort. It also empowers them with important health information, builds trust between physicians and patients, and encourages participation in future studies.
When sharing trial results, it's essential to present them in a way that includes everyone. This means translating findings into language that anyone can understand, regardless of their level of health literacy.
By closing the gap between the desire for information and its delivery, we can build a more informed and involved community, ultimately enhancing the impact of clinical research on public health.
References
- James Lind Institute. PATIENT INSIGHTS: The need for patient feedback (2020).
- Raza MZ, Bruhn H, Gillies K. Dissemination of trial results to participants in phase III pragmatic clinical trials: an audit of trial investigators intentions. BMJ Open 10, e035730 (2020).
- Bruhn H, Cowan EJ, Campbell MK, et al. Providing trial results to participants in phase III pragmatic effectiveness RCTs: a scoping review. Trials22, 361 (2021).
- Long, CR, Stewart MK & McElfish PA. Health research participants are not receiving research results: a collaborative solution is needed. Trials18, 449 (2017).
- National Institute for Health and Care Research (NIHR). Dissemination of results. Accessed here.
- Shelly CE, Logan C, Skorochod B, et al. Creating a best practice template for participant communication plans in global health clinical studies. Trials24, 158 (2023).
- NHS Health Education England (HEE). Ensuring decisions are underpinned by evidence from research (2022). Accessed here.
- NHS Health Research Authority. Communicating study findings to participants: guidance. Accessed here.
- Bruhn H, Campbell M, Entwistle V, et al. What, how, when and who of trial results summaries for trial participants: stakeholder-informed guidance from the RECAP project. BMJ Open12, e057019 (2022).
- Bidad N, MacDonald L, Winters ZE, et al. How informed is declared altruism in clinical trials? A qualitative interview study of patient decision-making about the QUEST trials (Quality of Life after Mastectomy and Breast Reconstruction). Trials17, 431 (2016).
- European Union. Good Lay Summary Practice (2021). Accessed here.
- FDA. Long-Term Follow-Up After Administration of Human Gene Therapy Products Guidance for Industry (2020). Accessed here.


.png)